Seasonal Respiratory Viruses
COVID-19, Influenza, Respiratory Syncytial Virus (RSV)
Who is at risk for seasonal respiratory virus infection?
Although everyone is at risk, the following are groups are at highest risk:
- Young children and the elderly
- People with compromised immune systems
- People with chronic diseases
- For more information on those at risk for severe disease:
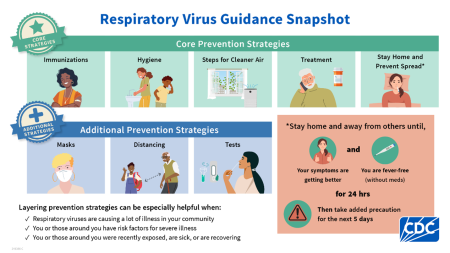
How to protect yourself
Vaccines are available for COVID-19, Influenza, and RSV.
- COVID-19 and influenza are approved for use for everyone 6 months of age and older. For the current recommendations:
- RSV immunizations are available for young children as some adults, including all adults 75 years and older. For the current recommendations:
To find vaccines talk to your healthcare provider or pharmacist or you can schedule an appointment at My Turn - California’s Vaccine Appointment Site.
What to do if I am sick
Do I need treatment for my respiratory virus infection?
- Most people can manage their symptoms at home.
- There are specific medications to treat Influenza and COVID-19 and if you are a person who is at increased risk for severe disease, talk to your healthcare provider about whether medications might help you.
When is respiratory season?
- In Orange County the respiratory virus season usually runs from fall to spring, although COVID-19 season continues to change.
- It is best to plan ahead and get vaccinated before the season starts.
Resources and Information for Providers
- California Department of Public Health
- COVID-19
- Influenza
- Respiratory Syncytial Virus (RSV)
Last Updated: 8/28/2025

